Consider exploring topics from across the top or click the More button on the right choosing information on foods, over the counter, or herbs. Use the pulldown menu to choose an item.Words in brown are links. This site contains details on cystic organ disease. If you cannot find what you are looking for, contact us, or try searching using the search engine or the language translator located at the bottom of each page.
BPA Bisphenol A, Plastic
Avoid BPA

BPA Bisphenol A, Plastic is a potent endocrine disruptor (Phthalates, plastic) that lines canned goods including aluminum cans and it is found in anything plastic. Even buying organic canned goods will not protect you in this instance. Plastic was original designed for use as hormone replacement. With the discovery of pregnant mare's urine or Premarin a new synthetic hormone was born. Plastic fell by the wayside. Its manufacturers had to scramble to find other uses for plastic. Its use has been linked (along with Genistein from soy) to infertility among our young.
The kicker is some plastic labeled BPA-free is also found to leach estrogen like molecules into the blood supply of humans. BPS or Tritan was thought to be a better alternative without leeching of estrogenic material. Eastman's product Tritan®, marketed to be completely free of estrogenic leaching, showed such activity. It is considered BPA free yet 81% of Americans have detectable levels of BPS in their urine. Research from the Centers for Disease Control and Prevention shows that more than 90% of Americans have BPA in their urine, probably because the chemical can leach from bottles and cans. Canned goods can be lined with plastic for ease of use.
Nearly all paper receipts are coated in BPA, and a new study finds that the carcinogenic chemical quickly contaminates the blood of anyone who handles one.
BPA (Phthalates, plastic) is controversial because it exerts detectable, hormone-like properties. Ovariectomized rats were given BPA in 1930 and found to have increases in estrogen. A 2010 report from the United States Food and Drug Administration (FDA) raised further concerns regarding exposure of fetuses, infants, and young children. In September 2010, Canada became the first country to declare BPA a toxic substance. The European Union and Canada, banned BPA in baby bottles.
Scientists took a closer look at the effects of DES and other endocrine disruptors, such as BPA, on the health of humans and animals. In 1991, experts from an array of disciplines gathered at the Wingspread Conference on the Precautionary Principle to discuss a growing body of evidence pointing to the harmful effects of chemical exposures on human and animal populations. The attendees issued a consensus statement:
"We are certain of the following: a large number of man-made chemicals that have been released into the environment, as well as a few natural ones, have the potential to disrupt the endocrine system of animals, including humans."
BPA Free is just as hazardous BPA free plastic has also been shown to leach hormone like molecules into the body. If one can, it is best to avoid all plastic with Polycystic Liver Disease.
Phthalates
Another name for BPA is phthalates. Phthalates are in shampoos, conditioners, and other cosmetics. The EWG has a database to search for cosmetics without parabens without phthalates. Liver cysts, breast cancer, and prostate cancer contains a common link. It is within the hormone receptor attached to the cell wall. The cell walls have hormone receptors and these cell walls incorporate molecules that look similar to hormones as true hormones, possibly triggering cyst growth, breast and prostate cancers. Some states have banned plastic bags.
What Makes Liver Cysts Grow?
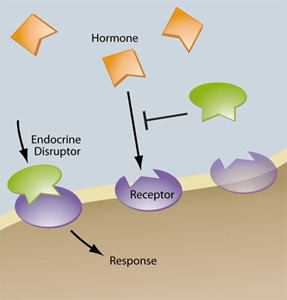
Liver cysts have receptors within their cell walls. These following compounds are similar. They ↑ liver size and cyst growth attaching to hormone receptors within the liver cysts.
BPA
Bleach
Endocrine disruptors
Hormones
Parabens
Phytoestrogens
Phthalates
Plastic
Xenoestrogens
Canned Food Raised Reporters' Bisphenol-A ↑ 2000%
Four Swedish reporters faced a savory (or unsavory) assignment: eat nothing but canned food for two days. The intrepid journalists enjoyed meals like canned beans and bacon or a tin of sardines for breakfast, served on plastic plates and accompanied by microwaved coffee in a plastic mug. For lunch they could have tuna salad assembled from ingredients that all originated in cans, or canned ravioli, washed down with beer from a can, and followed by canned fruit served on top of ice cream made from tinned evaporated milk. Yum. Svenska Dagbladet, the daily Swedish newspaper that orchestrated this experiment, to see how canned food affects BPA levels, counseled the journalists to follow their normal eating routines in the days leading up to the experiment, though on the final day before the 48 hours of canned food they attempted to eat "BPA-free."
The experiment, though not considered scientifically valid, was designed with the help of researchers from Lund University. After the two-day experiment, the newspaper team sent urine samples from the four reporters to Lund's lab. The results, showing pre- and post-urinalysis, shocked the team. All four of the experiment subjects had markedly increased levels of bisphenol A in their urine. The shocking part was that the levels (calculated as nanograms per milliliter) rose between 2,800 and 4,600 percent from the two days of eating nothing but canned. In Sweden and elsewhere, safe levels of BPA, an estrogen-like chemical widely used in plastic products, are still being debated. The Swedes have (since April this year) outlawed the use of BPA in food packaging for children under three. The Environmental Working Group lists ten studies showing BPA is harmful at current levels. But the US Food and Drug Administration has denied a recent petition from the Natural Resources Defense Council to have BPA outlawed from food packaging.
The FDA's conclusion: scientific evidence at this time does not suggest that the very low levels of human exposure to BPA through the diet are unsafe.
BPA Banned From Kids Food Packaging in Sweden
April 30th, 2012
Use of the chemical bisphenol A (BPA) has been banned in Sweden from all packaging intended to contain food and
other products for children, due to concerns about the substance"s effects on the body. The Swedish Chemical Agency
announced the BPA ban earlier this month, following a 2011 government report that indicated investigators were
unable to determine the levels at which BPA exposure could be deemed safe. The decision comes about one month after
the FDA decided to take no action on the chemical's use by the food packaging industry in the United States.
Swedish canned food and exposure in Swedish nursing women
4-Nonylphenol (NP) and bisphenol A (BPA) are phenolic substances used in high volumes by the industry. Studies on cells and in experimental animals have shown that both these compounds can be classified as estrogenic hormone disrupters. Information about the exposure of humans to NP and BPA is still scarce, especially regarding levels in human blood. The first aim of this study was to investigate possible sources of NP and BPA exposure from food, by analyzing the levels of NP and BPA from a Swedish food market basket, based on the Swedish per capita food consumption. A second aim was to investigate blood serum levels of NP and BPA, as well as NP-ethoxylates, among young women in Sweden (n=100). Moreover, associations between food consumption and blood NP and BPA levels were studied. In food, NP was to some extent found at levels above limit of quantification (LOQ 20ng/g fresh weight) in fruits, cereal products, vegetables, and potatoes. BPA levels above LOQ (2ng/g fresh weight) were found in fish, meats, potatoes, and dairy products. The estimated mean intakes per capita were (medium bound) 27ug NP/day and 3.9ug BPA/day, showing that food is a source of BPA and NP in the general Swedish population. In blood serum, free NP above limit of detection (LOD 0.5ng/g) was detected in 46% of the study participants while detectable levels of total NP (LOD 0.8ng/g) were observed in 43%. The corresponding percentages for BPA were 25% and 22%, respectively. The results indicate that there is a continuous source of exposure to NP and BPA that is high enough for free NP and BPA to be detected in some consumers. Among the participants with quantifiable levels of free and total NP (n=38), 85% (median, range: 38-112%) of the NP was present as free NP. For BPA 76% (49-109%) was detected as free BPA (n=15). All women had levels of ethoxylates of NP below LOD (0.1-0.7ng/g). A significantly higher total consumption of fruits and vegetables was reported in questionnaires by participants with NP levels at or above LOD than among women with levels below LOD. This result is supporting the market basket results of relatively high NP levels in these types of food.
Altered Carcinogenesis and Proteome in Mammary Glands of Rats after Prepubertal Exposures to the Hormonally Active Chemicals Bisphenol A and Genistein
Via our diet, we are exposed to numerous natural and man-made chemicals, including polyphenols with hormone-like properties. The most abundant hormonally active polyphenols are characterized as weak estrogens. These chemicals are hypothesized to interfere with signaling pathways involved in important diseases such as breast cancer, which in most cases is initially estrogen dependent. Two such chemicals are bisphenol A (BPA), a plasticizer, and genistein, a component of soy. In spite of both possessing estrogenic properties, BPA and genistein yield different health outcomes. The exposure of rats during the prepubertal period to BPA increases the susceptibility of adult animals for mammary cancer development, whereas genistein decreases this susceptibility in a chemically induced model. Because both BPA and genistein possess estrogenic properties, it is certainly plausible that additional mechanisms are affected by these chemicals. Hence, it was our goal to investigate at the protein level how exposure to these 2 chemicals can contribute to mammary cancer causation as opposed to cancer chemoprevention. Using 2-dimensional gel electrophoresis followed by MS analysis, we identified differentially regulated proteins from the mammary glands of rats prepubertally exposed to BPA and genistein. Following protein identification, we used immunoblotting techniques to validate the identity and regulation of these proteins and to identify downstream signaling proteins. Our studies highlight the importance of proteomics technology in elucidating signaling pathways altered by exposure to hormonally active chemicals and its potential value in identifying biomarkers for mammary cancer.
Unconjugated bisphenol A cord blood levels in boys with descended or undescended testes
The presence of uBPA in all CB samples suggests placental transfer and fetal exposure. Similar uBPA levels in the control and cryptorchid groups make the participation of fetal exposure to uBPA in the physiopathology of undescended testes unlikely. However, the observed nanomolar uBPA concentrations support assessment of epidemiological relationships between CB uBPA and other human diseases.
The Intersection of Neurotoxicology and Endocrine Disruption
Endocrine disruption, the guiding theme of the 27(th) International Neurotoxicology Conference, merged into the neurotoxicology agenda largely because hormones help steer the process of brain development. Although the disruption motif first attracted public health attention because of reproductive anomalies in both wildlife and humans, the neurobehavioral implications had been planted decades earlier. They stemmed from the principle that sex differences in behavior are primarily the outcomes of differences in how the brain is sexually differentiated during early development by gonadal hormones (the Organizational Hypothesis). We also now understand that environmental chemicals are capable of altering these underlying events and processes. Among those chemicals, the group labeled as endocrine disrupting chemicals (EDCs) offers the clearest evidence of such selectivity, a consequence of their actions on the endogenous sex steroids, androgens and estrogens. Two EDCs in particular offer useful and intriguing examples. One is phthalate esters. The other is bisphenol A. Both agents are used extensively in plastics manufacture, and are pervasive in the environment. Both are produced in immense quantities. Both are found in almost all humans. Phthalates are considered to function in essence as anti-androgens, while bisphenol A is labeled as an estrogen. Their associations with brain sexual differentiation are reviewed and further questions noted. Both EDCs produce a wider spectrum of health effects, however, than would be extrapolated simply from their properties as anti-androgens and estrogens. Obesity is one example. Further complicating their assessment as health risks are questions about nonmonotonic dose-response functions and about transgenerational effects incurred via epigenetic mechanisms. All these facets of endocrine disruption are pieces of a puzzle that challenge neurotoxicologists for solutions.
During the 1930's plastic was developed as an estrogen drug. Plastic is now known as an estrogen disruptor.
Release of bisphenol A from resin composite used to bond orthodontic lingual retainers
Accordingly, the potential toxicity of BPA from placing lingual bonded retainer might be negligible. On the other hand, because the health-effective amount of BPA is controversial, BPA release should be minimized.
Dental composite fillings and bisphenol A among children: a survey in South Korea
Having many dental composite filling surfaces on teeth may increase the urinary BPA concentration in children.
Expression of androgen, estrogen, progesterone, and growth hormone receptors in vascular malformations
Growth hormone receptor is over expressed and principally located in the vessels of vascular malformations. Growth hormone might contribute to the expansion of vascular malformations.
FDA makes it official, no BPA in baby bottles.
The FDA is officially putting a lid on bisphenol A (BPA) in baby bottles and sippy cups -- although industry has largely abandoned the plasticizer in these products already.The agency will still permit use of BPA in other food containers such as cans and water bottles, even as several manufacturers have voluntarily begun tagging their products as "BPA Free" in light of bad press.
Most Plastic Products Release Estrogenic Chemicals
Even BPA free plastic may also release estrogenic chemicals which can be harmful to severe PLD Polycystic Liver Disease.