



Words in brown are links. This site contains details on cystic organ disease. If you cannot find what you are looking for contact us or try the search engine or the language translator located at the bottom.
Proteinuria
Spilling protein in the urine is one of the first symptoms that we might possibly have PKD. Elevations in blood pressure is another symptom.
Slowing Progression of Kidney Disease: Focus on Proteinuria Reduction
From an interview with Dr. Brenner
How does protein stay on the serum side of the glomerulus and not empty into the urine?
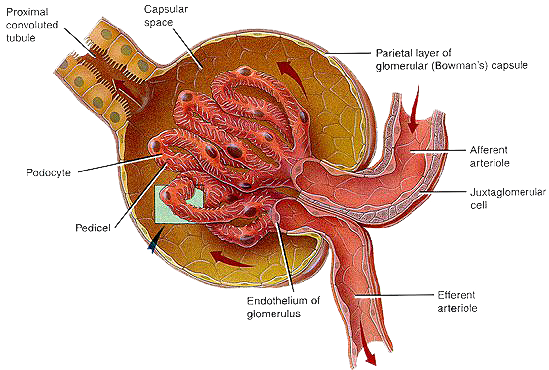
The glomerulus, enclosed in a capsule, Bowmans capsule, is the main filter of the nephron. The nephron is the functioning unit of the kidney. A tightly linked mesh of capillaries, make up the glomerulus of the kidney. Protein from the blood comes in contact with this linked mesh of capillaries. Studies show that these tightly l inked mesh of capillaries, making up the glomerulus, is what keeps the proteins albumin and immunoglobulin in the blood, and out of the urine. In addition, both the walls of the capillaries and the proteins that circulate in the blood are both negatively charged; so they naturally repel and this also prevents protein from passing through the glomerulus into the urine. It is this naturally repelling charge that further protects proteins from passing into the urine coupled with a tightly knit mesh of glomeruli capillaries. No one had previously appreciated this charge-and-mesh property.
When we see high protein levels in the urine, why has this typically tight barrier broken down?
Glomeruli have a charge-and-mesh property that is effected by an increase in pressure. Further studies demonstrated that, with proteinuria, the holes in the mesh get bigger and the negative charge disappeared. In the laboratory kidney disease was replicated by removing a kidney. This removes a large number of nephrons, which are made up of the filtering capillaries of the glomerulus and a tubular system essential for maintaining balance. Removing half of the nephrons causes the remaining nephrons to overwork, resulting in a progressively failing kidney. The more nephrons lost, the shorter the life span of the remaining kidney.
How do we slow disease progression?
Dr. Henry Christian, in 1913 prescribed low-protein diets. Lowering dietary protein enabled those with kidney disease to live longer. In the laboratory Dr. Barry Brenner
discovered that increasing dietary protein increases glomerular pressure, and the glomerulus works best under a lower pressure. Animal proteins or an excess dietary
proteins increases the kidney glomerular pressure. This increase in pressure causes circulating proteins to lose their negative charge and concurrently the linked
mesh of capillaries that make up the glomerulus becomes bigger allowing more proteins to pass through to the urine from the circulating blood. Perhaps this can help
explain how potassium citrate diminish proteinuria There have been clinical trials with potassium citrate concluding that it lowers pressure. As far back as 1913
we have known that low protein diets enable individuals with kidney disease to live longer, many were unwilling to follow such a diet. Doctors tried lowering
glomerular pressure through lowering blood pressure.
Luckily, Angiotensin Converting Enzyme Inhibitors (ACE Inhibitors) had just appeared. Kidney life was prolonged indefinitely by blocking the formation of Angiotensin II.
It took 8 years from Dr. Brenners rat experiments to confirm these findings in humans, but today renal patients worldwide are treated with ACE inhibitors. In 1957 the
late Dr. Mackenzie Walser took this further. By combining ACE inhibitors, low protein diets (0.3 grams/kilogram of body weight), alkalinity, correcting anemia,
supplementing with essential amino acids he has had success in halting end stage renal disease. If individuals only dropped the protein intake and took the essential
amino acids [Calwood Amines], 30% of individuals were affected positively. If they took ACE inhibitors 40% of individuals were affected. But with the combination of
both this figure jumped to 90% decrease in proteinuria. Dr. Walser discovered that serum albumin can be increased by eliminating dietary proteins and supplementing
with essential amino acids, useful for many dialysis patients.
Scientists took urine samples of the entire population of the city of Groningen, Netherlands and found that among 80,000 tested, 3000 people were discovered to have
protein in the urine. They identified a renal risk factor and are now working towards prevention. Their research has led to 39 papers published in 5 years on the
impact of microscopic amounts of protein in the urine. Dialysis and transplantation in the United States this year alone will cost $25 billion. Governments in 80%
of the world cannot afford dialysis or transplantation at all; for them kidney failure is fatal for most of their citizens.
Dr. Lin in China has a huge clinical trial from 17 centers testing ACE blood pressure medications or ARB (ACE receptor site blockers) along with low protein no
animal protein diets. Preliminary results are very good.

When kidney functioning diminishes.
Dr. Mackenzie Walser's book Coping with Kidney Disease
outlines a plan to try with your nephrologist:
Dialysis and transplantation in the United States this year alone will cost $25 billion. In the USA for a single patient, the estimated cost of dialysis is $75,000 per year. The cost
of transplant surgery and care is $100,000, with an additional $10,000/year in anti-rejection medication costs. Eighty Percent of the world governments cannot afford dialysis
or transplantation at all. For those with kidney failure this diagnosis is fatal. Dr. Lin in China has a huge clinical trial from 17 centers testing ACE blood pressure
medications or ARB (ACE receptor site blockers) along with low protein no animal protein diets.
One article from the pulldown menu below suggests that controlling glomerular hypertension limits kidney injury in the animal model. Renal ablation is accompanied by
structural lesions and further suggests that sustained single nephron hyperfiltration may have maladaptive consequences by damaging remnant glomeruli.
Written in 2001, Dr. Brenner commented that it took 8 years from his laboratory results to be translated into care options for humans with kidney disease.
Proteinuria Can ↓ Life Expectancy
Proteinuria is a marker of kidney disease and is associated with risk of adverse outcomes. In Canada we studied 812,386 individuals. In conclusion, we found a substantial and progressive decrease in life expectancy for men and women with the presence and severity of proteinuria.