|
LIVER TRANSPLANT SURGERY
 Choose a liver transplant article from ABOVE
Choose a liver transplant article from ABOVE
|
 Live donor liver transplantation (LDLT) is a where a living person donates a portion of liver to another. The feasibility of LDLT was first demonstrated in the United States in 1989. The recipient was a child, who received a segment of his mother's liver. Since that time, LDLT for children has enjoyed wide success and many pediatric programs use this technique.
In the pediatric experience, survival of both the recipient and the transplanted liver (graft) at one year is about 90%. Donor complications have been very few. A rising population of adult patients awaiting liver transplantation has led to the application of LDLT for adult patients, and the preliminary results have been very encouraging. Only a handful of centers in this country perform the procedure. For more information on living donor transplant click here. This has links to what constitutes a good donor, how is the operation performed. Live donor liver transplantation (LDLT) is a where a living person donates a portion of liver to another. The feasibility of LDLT was first demonstrated in the United States in 1989. The recipient was a child, who received a segment of his mother's liver. Since that time, LDLT for children has enjoyed wide success and many pediatric programs use this technique.
In the pediatric experience, survival of both the recipient and the transplanted liver (graft) at one year is about 90%. Donor complications have been very few. A rising population of adult patients awaiting liver transplantation has led to the application of LDLT for adult patients, and the preliminary results have been very encouraging. Only a handful of centers in this country perform the procedure. For more information on living donor transplant click here. This has links to what constitutes a good donor, how is the operation performed.
HOW LONG WILL A LIVER TRANSPLANT LAST?
A study of over 2702 liver transplants in the UK showed for women it was 26 years.
ALTRUISTIC DONORS NEEDED
Take a few moments to read this article. It is dedicated to Anne and others with PLD. This next article was sent by Judie, relates the story of woman who happily traded her 46 pound cystic liver for a transplanted organ. A recent article from Hong Kong Rapid Liver Donor Workup, When Altruism Is High, Gets Organs has resulted in an increase in liver organs for transplant.
|
BLOODLESS LIVER TRANSPLANT PERFORMED World's First Adult-to-Adult Live Donor Liver Transplant Without a Blood Transfusion - June 15, 1999
Some said it could not be done. Others simply refused to attempt it. But Bill Jennings needed a liver transplant and he needed the procedure to be performed without the transfusion of blood or blood products. Neither his end-stage liver disease nor his religious beliefs as a Jehovah's Witness would allow for anything less.
Jennings already had a donor lined up: his older brother Scott, who was both able and willing. The problem was finding a doctor who would give Jennings a chance at a normal and healthy life while still respecting his religious convictions.
Left Picture: To lower the risk of bleeding both before and during surgery, a transjugular intrahepatic portal systemic (TIPS) shunt is inserted into the portal vein via the internal jugular vein.
Right Picture: The shunt reduces pressure in the portal vein and in distended veins.
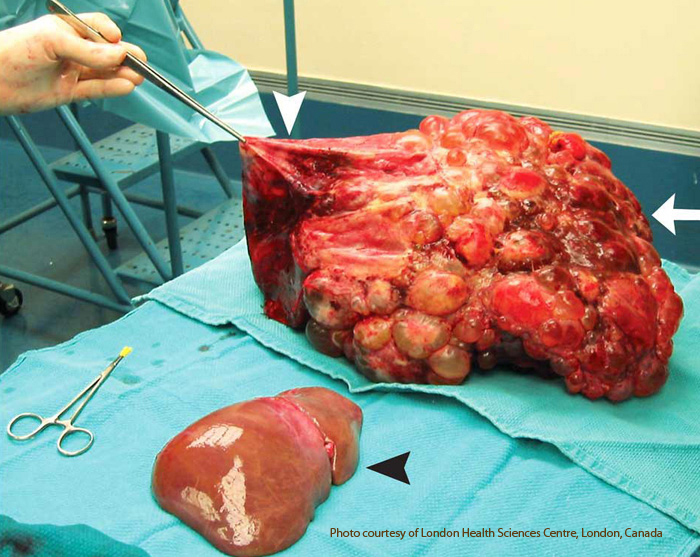
Polycystic liver is at the top between the white arrows. The polycystic liver has been decompressed. It was even larger before the decompression. The black arrow indicates a normal size liver.
LIVER TRANSPLANT FOR PLD - April 12, 2007 New England Journal of Medicine. A 51-year-old woman with polycystic liver and kidney disease had undergone renal transplantation 21 years before presentation. She had no evidence of cerbrovascular malformations. Bother her father and aunt also had polycystic kidney disease. After the renal transplantation, her liver had become progressively diseased and enlarged through cystic changes. Early satiety, malnutrition, and abdominal pain necessitated a liver transplantation. The recipient's weight at transplantation was 59 kg. A 9.1-kg liver (white arrow) was removed and replaced with a whole graft that was one tenth the weight of the diseased liver (black arrowhead). A large cyst at the dome of the native liver had to be decompressed (white arrowhead) to allow for access to the recipient's supra hepatic vena cava. She made an excellent recovery and had normal kidney and liver function at 4 years of follow-up.
PLD Liver Dialysis - Jan-Feb 2004 liver dialysis has now become available on a limited basis. According to Hepatitis central it has received FDA approval. Some sites offering liver dialysis include:
• Tulane
• University of Tennessee-Bowld
• University of Texas- San Antonio
• Loyola University
• University of Iowa
• California Pacific Medical Center
• University of California at San Diego
• New York University
• Oklahoma City
• Mayo Clinic Arizona, Jacksonville, Rochester and more
Liver dialysis is only for short term use according to this article
LIVER TRANSPLANT FOR PLD has (2) possibilities: a cadaver transplant and a living donor transplant. Cadaver transplants are difficult to obtain, because usually PLD polycystic liver disease livers do not fail, but they can become life threatening. I report the following to pass onto to transplant centers to help move you up the waiting list for a cadaver transplant. Several individuals have died from PLD. It is indeed a life threatening illness. One was a woman in Japan. She had massive liver cysts. The doctors told her cystic livers never fail and there was nothing to do. Her liver continued to enlarge and grow until (as many of us have noted) the bones of the ribs began becoming slightly deformed. Eventually one of her ribs cracked. The broken rib pierced her bowel and she died from septicemia, blood poisoning. Another individual developed HVOO, hepatic venous outlet obstruction. Blood from the body in the inferior vena cava (the biggest vein in the body) became more and more obstructed until it began to clot and she died. A gentleman I knew developed severe emaciation and muscle wasting. Everything he ate came back up. There was no room for his compressed stomach nor his intestine to absorb any nourishment from the food. They gave him feedings via a stomach tube. They tried to feed him hyperalimentation through a big blood vessel. Eventually he died of malnourishment and total body shut down.
There was another death from PLD. A woman 50 y/o developed an infection within the liver cyst. The doctors tried very hard to clear up this infection and were unsuccessful. She was in Greece and died from liver failure directly related to her cystic liver.
I do not report any of this to frighten anyone. I say it to add to our collective knowledge about this disease. It upsets me terribly when I hear of individuals being told there is nothing to do.
The diagnoses of liver cysts can occur in childhood and even prenatally, especially when ARPKD is present – a recessive form of PKD polycystic kidney disease. With this disease, it too is most commonly found in children, but not always. I have communicated with a woman who discovered ARPKD as an adult. She was 37. Just recently, we received word that Joe, age 67, received a dual transplant, kidney and liver, from Omaha, Nebraska. Congratulations Joe!
The FDA has issued a warning on the use of sirolimus in liver transplants.
|