 |
ADPLD – POLYCYSTIC LIVER DISEASE – ADPKD with PLD Listen to this excellent lecture now on
PLD polycystic liver disease
by Dr. Vicente Torres given June 15, 2004 at the PKD conference. Some information on this page were derived from
collected experiences of individuals with PLD polycystic liver disease.
Proton pump inhibitors and H2 blockers are useful for GERD which
may also block the release of secretin, a hormone that triggers
the expansion and filling of liver cysts with fluid.
|
|
|
Jan 2004 LIVER DIALYSIS has received FDA approval for short term use. |
POLYCYSTIC LIVER AT THE TOP WITH THE WHITE ARROWS. THIS POLYCYSTIC LIVER HAS BEEN DECOMPRESSED. IT WAS EVEN LARGER BEFORE THE DECOMPRESSION. THE BLACK ARROW INDICATES A NORMAL SIZED LIVER.
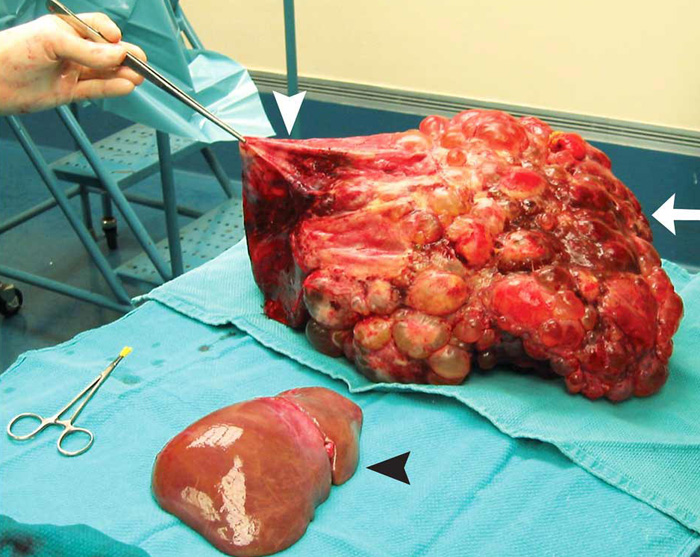
LIVER TRANSPLANT FOR PLD from the April 12, 2007 New England Journal of Medicine. A 51-year-old woman with polycystic liver and kidney disease had undergone renal transplantation 21 years before presentation. She had no evidence of cerbrovascular malformations. Bother her father and aunt also had polycystic kidney disease. After the renal transplantation, her liver had become progressively diseased and enlarged through cystic changes. Early satiety, malnutrition, and abdominal pain necessitated a liver transplantation. The recipient's weight at transplantation was 59 kg. A 9.1-kg liver (white arrow) was removed and replaced with a whole graft that was one tenth the weight of the diseased liver (black arrowhead). A large cyst at the dome of the native liver had to be decompressed (white arrowhead) to allow for access to the recipient's supra hepatic vena cava. She made an excellent recovery and had normal kidney and liver function at 4 years of follow-up.
LIVER TRANSPLANT FOR PLD has
(2) possibilities: a cadaver transplant and a living donor transplant. Cadaver
transplants are difficult to obtain, because usually PLD polycystic liver
disease livers do not fail, but they can become life threatening. I report
the following to pass onto to transplant centers to help move you up the
waiting list for a cadaver transplant. Several individuals have died from
PLD. It is indeed a life threatening illness. One was a woman in Japan. She
had massive liver cysts. The doctors told her cystic livers never fail and
there was nothing to do. Her liver continued to enlarge and grow until (as
many of us have noted) the bones of the ribs began becoming slightly deformed.
Eventually one of her ribs cracked. The broken rib pierced her bowel and
she died from septicemia, blood poisoning. Another individual developed HVOO,
hepatic venous outlet obstruction. Blood from the body in the inferior vena
cava (the biggest vein in the body) became more and more obstructed until
it began to clot and she died. A gentleman I knew developed severe emaciation
and muscle wasting. Everything he ate came back up. There was no room for
his compressed stomach nor his intestine to absorb any nourishment from the
food. They gave him feedings via a stomach tube. They tried to feed him hyperalimentation
through a big blood vessel. Eventually he died of malnourishment and total
body shut down.
There was another death from PLD. A woman 50 y/o developed an infection within
the liver cyst. The doctors tried very hard to clear up this infection and were
unsuccessful. She was in Greece and died this past November from liver failure
directly related to her cystic liver.
Each of you continue to seek help. Continue to look for answers. I do not report
any of this to frighten anyone. I say it to add to our collective knowledge
about this disease. It upsets me terribly when I hear of individuals being
told there is nothing to do. 90% of individuals with PKD have liver cysts.
It is the severe form that we seek treatment for. The diagnoses of liver cysts
can occur in childhood and even prenatally, especially when ARPKD is present –
the recessive form of PKD polycystic kidney disease. With this disease, it
too is most commonly found in children, but not always. I have communicated
with a woman who discovered ARPKD as an adult of 37.There is plenty
to do, especially at the early stages of PLD polycystic liver disease.
ALTRUISTIC DONORS NEEDED Take a few moments to read this article. It is dedicated to Anne and Leo who died while awaiting a liver transplant. This next article was sent by Judie. It relates the story of woman who happily traded her 46 pound cystic liver for a transplanted organ. A recent article from Hong Kong Rapid Liver Donor Workup, When Altruism Is High, Gets Organs has resulted in an increase in liver organs for transplant.
HOW LONG WILL A LIVER TRANSPLANT LAST? A study of over 2702 liver transplants in the UK showed for women it was 26 years.
WHERE IN THE USA CAN I GO FOR A LIVER TRANSPLANT? There are many great transplant centers located around the USA. One that seems to stand out in helping us PLD'rs is the Mayo Clinic in Jacksonville, Florida. Head of the liver transplant team is Jeffery L. Steers M.D. Department of General Surgery/Liver Transplantation, Mayo Clinic Jacksonville, FL. If you need a liver resection or wish to be assessed to see which procedure is best for you, V. Torres M.D. Department of Nephrology at the Mayo Clinic in Rochester, Minnesota is the place to go. To listen to a lecture by Dr. Torres on PLD, click here.
FROM A FRIEND FOLLOWING A SUCCESSFUL PLD LIVER TRANSPLANT UK It is over 16 months since I had my transplant and am continuing to do so very well. People I talk to can not believe that I have recovered so quickly over such a short period of time. If you recall I did do a lot of leg work before it all happened. It took a year and a half after I was diagnosed to get acceptable treatment. I did get a lot of help from you, and peoples information on the PKD support. I also kept asking for second opinions which involved me traveling over the country to find specialists who I could relate to. I remember talking to you for ages about treatment and getting a high because you gave me hope after such a lot of negative feedback. I ended up at the Queen Elizabeth in Birmingham because they told me the truth and were willing to help me. When I went on the list for transplant I was fortunate to have blood group A+ which is the best one to be for transplant purposes. The worst one is 'O' because more people are this and consequently there is more demand for organs. I knew that there was at least one before me because she was already waiting in the hospital. So when I went in for transplant (only 10 days later) she had already had the transplant. I know for a fact that she is still having problems whilst I only had a set back the second day after my operation and they gave me drugs to combate any rejections. The Doctor said it looked good if the problems occurred straight away and I stood a very good risk of it all being a good transplant. Well he seems to have been right so far.
FROM A FRIEND WAITING FOR PLD LIVER TRANSPLANT FROM DR. JENKINS Turned on my TV this morning and there smiling back at me was my liver transplant surgeon, Dr. Jenkins from Lahey Clinic in Burlington, MA.....seems like the liver team at Lahey was about to complete a rare transplant surgery... a new kidney and liver will be transplanted from 2 live donors setting the stage for a complicated triple surgery. The woman has a rare auto-immune disease that destroyed her liver and kidney (they didn't say what the disease was). The woman's uncle is donating part of his liver and her cousin is giving a kidney. Transplanting organs from healthy people is complicated; but, three simultaneous high risk surgeries is leading-edge technology. The team will occupy three of the hospital's operating rooms and there will be about 40 doctors, nurses, and other technicians.

Live
donor liver transplantation (LDLT) is a procedure in which a living person donates
a portion of his or her liver to another. The feasibility of LDLT was first
demonstrated in the United States in 1989. The recipient was a child, who received
a segment of his mother's liver. Since that time, LDLT for children has enjoyed
wide success and many pediatric programs use this technique.
In the pediatric experience, survival of both the recipient and the transplanted
liver (graft) at 1 year is about 90%. Donor complications have been very few.
A rising population of adult patients awaiting liver transplantation has led
to the application of LDLT for adult patients, and the preliminary results have
been very encouraging. Only a handful of centers in this country perform the
procedure. For more information on living donor transplant click
here. This has links to what constitutes a good donor, how is the operation
performed and more.
BLOODLESS LIVER TRANSPLANT PERFORMED
World's First Adult-to-Adult Live Donor Liver Transplant Without a Blood Transfusion
- June 15, 1999
Some said it could not be done. Others simply refused to attempt it. But Bill
Jennings needed a liver transplant and he needed the procedure to be performed
without the transfusion of blood or blood products. Neither his end-stage liver
disease nor his religious beliefs as a Jehovah's Witness would allow for anything
less.
Jennings already had a donor lined up: his older brother Scott, who was both
able and willing. The problem was finding a doctor who would give Jennings a
chance at a normal and healthy life while still respecting his religious convictions.
For Jennings, then 44, the father of two and owner of a computer business in
Parker, Arizona, this was yet another bump in a road that had begun 20 years
earlier with a diagnosis of primary sclerosing cholangitis or PSC. This rare,
debilitating disease is associated with a narrowing and inflammation of the
liver's bile ducts, eventually leading to cirrhosis of the liver. No one really
knows what causes PSC and its resulting cirrhosis--a lack of understanding that
frustrated Jennings, who does not smoke and only drank alcohol in moderation.
And the only known cure is liver transplantation.
By the beginning of January, 1999, Jennings' condition had taken a turn for
the worse. His disease had progressed and he had developed severe jaundice,
his light skin taking on a deeply tanned hue. He could no longer work in his
computer shop, and could neither sit nor stand for long periods of time. He
then contacted three liver specialists in Northern California, where his mother
lived. All declined to perform a bloodless version of the transplant he so desperately
needed.
Finally, a family friend from Orange County who was a member of the L.A./Orange
County Hospital Liaison Committee for Jehovah's Witnesses pointed Jennings in
the direction of Randy B. Henderson, manager of the USC Transfusion-Free Medicine
and Surgery Program. Henderson set up an appointment for Jennings to see hepatobiliary
specialists Rick Selby, M.D., and Nicolas Jabbour, M.D.
On June 15, 1999, Jennings and the USC team made history by taking part in the
first-ever live donor liver transplant without a transfusion of blood or blood
products.
The Power of Their Convictions
Jehovah's Witnesses are prohibited from the use of blood and blood products
because of their acceptance of the Bible as "the inspired word of God,"
explains Henderson. "Based on several passages in both the Old and New
Testament that refer to 'eating' blood and 'abstaining' from blood, they do
not accept whole blood or major components-red cells, white cells, platelets
or plasma."
But Jehovah's Witnesses are not the only people who are interested in, or even
demand, bloodless alternatives. An increasing number of people are rejecting
the use of blood for an increasing number of valid reasons. In addition, notes
Jabbour, who is both medical director of the Program and associate director
of abdominal organ transplantation at USC University Hospital, there are an
increasing number of reasons for physicians themselves to consider bloodless
alternatives, even if the patient has no objections to the use of blood products.
"Blood products are useful but carry their own set of risks," says
Jabbour. "Thus, whenever we can avoid using them, we should not only in
Jehovah's Witness patients, but in every patient."
Bill Jennings was lucky in that he had the luxury of time. He needed the transplant,
of course, and he needed it quickly. But there was time enough to build up his
blood levels--in particular, his stores of red blood cells--so that his body
could afford to lose some blood during what was sure to be a risky surgery.
Blood has three main cellular components: red cells, white cells and platelets.
The percentage of red cells in the blood is measured by hematocrit levels: The
normal hematocrit value in an adult man is around 45 percent. Jennings' had
dropped to as low as 17. Before they would operate, the USC surgeons wanted
to see that boosted to the 45 percent range.
Several things were done to increase his levels. First, blood tests were used
sparingly. Second, Jennings was given supplemental iron and folic acid, and
a synthetic medication similar to erythropoietin, a hormone-like substance
produced by the kidneys that stimulates the bone marrow to produce red blood
cells. Those synthetic medications, Epogen or Procrit, are like naturally produced
erythropoietin and have the same effects.
The interventional radiologists, led by Michael Katz, M.D., also placed a transjugular
intrahepatic portal systemic (TIPS) shunt inside Jennings' liver. Patients with
advanced liver disease tend to have dangerous increases in pressure in the veins
flowing into the organ; because of the increased pressure, these vessels tend
to bleed. A TIPS shunt decreases the pressure in the portal vein, reducing the
risk of bleeding both before and during surgery.
Used all together, these techniques were a rousing success. By the day of his
surgery, Jennings' hematocrit levels had hit 45 percent. He was ready to go.
Transjugular Intrahepatic Portal Systemic Shunt (TIPS)
Above: To lower the risk of bleeding both before and during surgery, a transjugular
intrahepatic portal systemic (TIPS) shunt is inserted into the portal vein in
the liver via the internal jugular vein.
Below: The shunt reduces pressure in the portal vein and in distended veins--varicosities--nearby.
Assisting With Anesthesia
Getting Jennings'
hematocrit levels up high enough was only the first step in ensuring a successful
procedure. The next step was to have a series of reliable and efficient blood
management techniques to deal with the inevitable bleeding during the surgery-a
task that fell to a USC anesthesiology team of Earl Strum, M.D., Pajesh V. Patel,
M.D., and Duraiyah Thangathurai, M.D.
One of these techniques is an approach called acute normovolemic hemodilution,
in which the patient's whole blood is collected immediately prior to surgery,
and the rest of the blood is diluted with non-blood products such as normal
saline or other intravenous solutions. "Consequently," notes Patel,
an associate professor of anesthesiology, "if the patient bleeds during
surgery, he is bleeding diluted blood." Once the operation is completed,
the patient receives the concentrated blood that was collected prior to surgery.
But because Jehovah's Witnesses do not donate or store their own blood, this
technique needed to be tweaked in order to be used in the Jennings transplant.
To address this, Strum--who serves as interim chair and associate professor
in the Department of Anesthesiology, and also holds an appointment with the
Department of Orthopaedics--used an innovative device that keeps the collected
blood in circuit with the patient. "Since there is still a connection with
the body, the collected blood can be transfused back into the patient,"
Strum notes. "This allows Jehovah's Witness patients to observe their
religious beliefs concerning blood products."
A second useful technique involves a device called a "cell saver."
A cell saver does precisely that: It collects the patient's blood as it is lost
during surgery, cleans it and returns it to the patient. This is acceptable
to most Jehovah's Witnesses, says Henderson, because, like the bypass procedure,
it "can be viewed as an extension of their circulatory system. The belief
is that since the Bible does not specifically comment on these products or
equipment, it is left up to each individual to make a conscientious and informed
decision."
Finally, doctors working on a bloodless procedure like Jennings’ can give
the patient drugs to reduce his blood pressure. This is called hypotensive anesthesia,
explains Thangathurai, a professor of anesthesiology who also holds appointments
with the departments of surgery and urology. Lowering blood pressure decreases
the amount of bleeding that results when blood vessels are cut. "This approach
has been especially effective in urology cancer patients," notes Thangathurai.
The Careful Cut
Jennings and his
brother, Scott, underwent surgery on Tuesday, June 15th, at 7:30 a.m. The transfusion-free
surgical team, under the leadership of Selby, Jabbour and Yuri Genyk, M.D.,
first removed a segment of Scott's healthy right liver lobe along with the vessels
supplying blood to that segment. Jennings' diseased liver was then removed and
replaced by the donated healthy segment.
"Bloodless surgery does not require any special instrument or fancy technical
changes," Jabbour explains. "All it requires is being meticulous
as far as preventing blood loss when we are dissecting the tissue, and knowing
how to control the bleeding decisively using sutures and electrocoagulation.
Contrary to the image of the 'macho, aggressive, fearless' surgeon, one must
be precise and gentle."
"We take our time when performing these major surgeries, including liver
transplantation and liver resection," adds Selby. "Through a very
careful, calculated approach, we can control the blood flow. Both Scott and
Bill Jennings came through their surgeries beautifully. And just eight weeks
later, Selby reported, both liver halves, through the organ's natural regenerative
ability, had grown to normal size.
"I received excellent care from the surgical team," Jennings said
in an interview following the surgery, "and was extremely impressed with
their skill and willingness to treat me while respecting my religious convictions."
L.A. MOM HAD DUAL ORGAN TRANSPLANT Dual
Organ
By Tom Harrigan, Associated Press Writer - March 24, 2001
LOS ANGELES (AP) - When her children offered their own organs to save
her life, Maria Alvarez was terrified - not for herself but for them. The 57-year-old had been on dialysis for 31/2 years after kidney failure, and
her liver was more than twice normal size and barely functioning due to polycystic
disease. Fluid from the liver had already caused one infection that had nearly
killed her. But despite the pain, Alvarez was reluctant when doctors told her
that dual transplants - a kidney from Rosario Proscia, 34, and part of the liver
of son Jose Alvarez, 36 - could help her become healthy again.

WHAT ARE SYMPTOMS OF PLD?
Most
individuals do not experience any symptoms from their liver cysts. A number
of individuals have multiple liver cysts which can cause many symptoms. At
the age of twenty or so if individuals with cystic livers have only one or
two liver cysts, more than likely they will not go on to develop the kind
of cystic livers which require medical intervention. Some symptoms may include:
back
pain
bleeding into a cysts
candidiasis or yeast
clots in blood vessels from pressure of cystic liver
collapse lung
craving for sweets
difficulty breathing when laying flat
discomfort and fullness
distortion of ribs
disturbed sleep
early satiety
emaciated
fatigue
fat loss
fluid in the lung
fractures of ribs
headache
hemorrhoids
itchy skin
liver cyst rupture
liver cyst infection
inability to fall asleep
massive belly from cystic liver
massive liver presses against veins and arteries
matted spider veins telangectasias that burn
muscle wasting
nausea
pain
poor appetite
rupture of a liver cysts presents like an acute abdomen
rarely bones are broken from the growth of liver cysts
really hungry but unable to eat more than a cupful with a feeling of fullness
and discomfort
reduced platelets that are of no significance
shortness of breath especially when walking
skinny upper body
sleeping flat on back difficult
swelling of legs, feet
swelling of the feet that makes walking painful
tiredness-from carrying around an extra 40 pounds of cystic organs
unable to walk very far
urinary stress incontinence
uterine prolapse
varicose veins
weight gain
WHAT ARE SOME SURGICAL TREATMENTS
FOR PLD?
Liver
resection, liver transplant, liver
artery ablation, To read more liver treatments click
here.
Liver
Dialysis
A
Jan-Feb 2004 article has shown that liver dialysis
has now become available on a limited basis. According to Hepatitis central
it has received FDA approval:
Sites include:
• Tulane
• University of Tennessee-Bowld
• University of Texas- San Antonio
• Loyola University
• University of Iowa
• California Pacific Medical Center
• University of California at San Diego
• New York University
• Oklahoma City
• Mayo Arizona, Jacksonville, Rochester and more
Liver dialysis is only for short
term use according to this article.
Wondering if it might be useful when coupled with a liver resection until
the remnant of the liver kicks and starts working?
LIVER HERBS
Herbs – organic milk thistle,
turmeric, artichoke, & saffron
There
are a few liver herbs that I have tried and found helpful. I use organic milk
thistle plus (milk thistle, turmeric, and artichoke). I took three tablets
3 times a day. I also take saffron infusion whenever I have a liver ache and
this relieves it immediately. I take 1/4 teaspoon of organic saffron in a
cup of water and allow it to simmer on the stove until a half cup of liquid
remains. I then strain it and sip it. This costly herb is available through
vanilla saffron imports
for $35 for huge tin.
Intensive research into the liver-protecting )hepatoprotectant) properties of milk thistle and the responsible components, the mechanism of action began in earnest 30 years ago. University of Munich H. wagner was successful in isolating a compound named silymarin. It is a mixture of different flavonolignans including silybinin, silybinin, and silychristin. Clinical trials in Europe, primarily Germany have shown the efficacy of silymarin in the treatment of metabolic liver damage, chronic hepatitis, and bile duct inflammation. Hepatoprotective effects have been demonstrated by accelerating normalization of impaired liver function. Accelerated improvement in serum levels of GOT, GPT, GT and bilirubin. I have noted that my metabolism of estrogen has returned to normal. For more information download this article and read about milk thistle, turmeric, artichokes and saffron.
POLYCYSTIC LIVER DISEASE MEDICAL RESEARCH PROJECT This is an ongoing project. If you have no kidney cysts and no family members have kidney cysts, then you probably have ADPLD, autosomal dominant polycystic liver disease. I realize it is very confusing. If you need further clarification, send an email. A friend Lyn has established a PLD polycystic liver disease support list serve. None of her family members have kidney cysts. Any individuals without kidney cysts and only liver cysts, there is an ongoing study from the Mayo with Dr. Peter Harris and Dr Torres and at Yale with Dr. S. Somlo all looking to do gene phenotyping of ADPLD. This requires a donation of a test tube of your blood. It does not require travel. They can mail the kit to you and you mail it back in a pre-paid envelope. Email with questions. If you would like to contact Dr. Somlo directly click here.
OCTREOTIDE Clinical trials will be completed April 2010. This is the first clinical trial to diminish liver cysts.
LIVER TRANSPLANT (to
download click the underlined links)
Surgical management of polycystic
liver disease
Massive hepatomegaly can lead to disabling symptoms of
abdominal pain, early satiety, persistent nausea, dyspnea, ascites, biliary
obstruction, and lower body edema. Earlier transplantation in appropriate candidates
would seem to offer a greater chance of improved outcomes, meaningful recovery,
and return to their prior functional status and quality of life. These patients
had severe anorexia, physical exhaustion, and evidence of malnutrition from
end-stage PCLD for liver transplant for APLD.
Polycystic liver disease: multimodality
imaging for complications and transplant evaluation.
Cyst fenestration with
partial hepatic resection and liver transplantation are two therapies that
provide more permanent resolution of symptoms in patients with extensive hepatic
involvement. Help the radiologist provide the referring clinician with important
information for therapeutic decision making. RSNA, 2006.
Liver and kidney transplantation
for polycystic liver and kidney-renal function and outcome.
Transplantation
is an excellent option for PLD with dramatic improvement in quality of life
and acceptable morbidity. acceptable renal function at time of transplantation,
solitary liver transplantation has an excellent outcome.
Liver transplantation
in polycystic liver disease: A relevant treatment modality for adults?
We conclude
that patients treated for PLD by LTX have a good long-term prognosis and excellent
relief of symptoms and that LTX might be considered in severe cases of PLD,
where conventional surgery is not an option.
Results of percutaneous sclerotherapy
and surgical treatment in patients with symptomatic simple liver cysts and
polycystic liver disease.
Results of percutaneous sclerotherapy and surgical
treatment for PLD are disappointing.
Outcome and Quality of Life in Patients
With Polycystic Liver Disease After Liver or Combined Liver-Kidney Transplantation.
Patients with advanced polycystic liver or polycystic liver-kidney disease
have an excellent survival rate and an improved quality of life after liver
or combined liver-kidney transplantation.
New advances in evaluation and management
of patients with polycystic liver disease.
In these patients, medical management
alone has proved ineffectual. Therefore, in the symptomatic APLD patient, surgical
therapy remains the mainstay of therapy and includes cyst aspiration and sclerosis,
fenestration with and without hepatic resection and orthotopic liver transplantation.
Successful transplantation of cadaveric polycystic
liver: case report and review of the literature. We report the successful
use of a polycystic donor liver and review the experience with this donor population.
We propose that the selective use of polycystic donor livers containing small
(<5 cm) cysts with preserved
liver parenchyma is safe and appropriate.
Quality of Life and Liver Transplantation
in Patients With Polycystic Liver Disease.
Chronic and end-stage liver diseases
negatively affect many aspects of patients’ physical functioning and
quality of life. A considerable amount of research in the past few decades
has been devoted to the measurement of HRQL. Global (generic) aspects of health-related
quality of life are commonly assessed, which allows for comparisons between
patients with different diseases.

last updated Wednesday, August 10, 2011 8:17 PM