Articles Potassium Citrate & Alkalinity




Nephron Physiol. 2003 Jan;93(1):P14-20.
Tanner GA, Tanner JA.
Source
Department of Cellular and Integrative Physiology, Indiana University School of Medicine,
Indianapolis, Ind 46202, USA
Abstract
J Am Soc Nephrol. 1998 Jul;9(7):1242-8.
Tanner GA
Source
Department of Physiology and Biophysics, Indiana University School of Medicine, Indianapolis 46202, USA.
Abstract
Sakhaee K, Pak C.
Department of Internal Medicine, University of Texas Southwestern Medical Center, Dallas, Texas; Center for Mineral Metabolism and Clinical Research, University of Texas Southwestern Medical School, Dallas, Texas.
PKD 'rs who wish to eat vegan, this is very healthy. But for those who want to continue to eat meat, there is always orange juice, melon juice, or potassium citrate to bring the body toward alkaline. If potassium salts are ever needed (post transplant or while on diuretics), potassium citrate might be a better choice. The trick is to find a citrate salt that is palatable.
Calcium supplementation is commonly recommended for patients after Roux-en-Y gastric bypass to avert bone loss. To test the hypothesis that effervescent (liquid) potassium-calcium-citrate (PCC) might be more bioavailable than a tablet formulation of calcium citrate (Citracal Petite), the present study compared a single dose response of the 2 compounds. The present study was conducted at the University of Texas Southwestern Medical School at Dallas.
METHODS:
A total of 15 patients who had undergone Roux-en-Y gastric bypass were included in a 2-phase, crossover, randomized study comparing the single-dose bioavailability of PCC versus Citracal Petite. After following a restricted diet for 1 week, the participants ingested either a single dose of 400 mg elemental calcium as PCC or Citracal Petite. Sequential serum and urine samples were collected for a 6-hour period after the dose and analyzed for calcium, parathyroid hormone, and acid-base parameters.
RESULTS:
Compared with citracal petite, PCC significantly increased the serum calcium concentrations at 2, 3, and 4 hours after the oral load. The peak to baseline variation and increment in serum calcium (area under the curve) were significantly greater after PCC (P = .015 and P = .002, respectively). Concurrently, the baseline to nadir variation and decrement in serum parathyroid hormone (area over the curve) were significantly greater after PCC (P = .004 and P = .005, respectively). Moreover, compared with Citracal Petite, PCC caused a significantly greater increment in urinary citrate (P < .0001) and potassium (P = .0004) and a significantly lower increase in urinary ammonium (P = .045).
CONCLUSION:
In patients who have undergone Roux-en-Y gastric bypass, PCC was superior to Citracal Petite in conferring bioavailable calcium and suppressing parathyroid hormone secretion. PCC also provided an alkali load.
Int Braz J Urol. 2011 Sep-Oct;37(5):611-6.
Lojanapiwat B, Tanthanuch M, Pripathanont C, Ratchanon S, Srinualnad S, Taweemonkongsap T, Kanyok S, Lammongkolkul S.
Source
Division of Urology and Department of surgery, Chiangmai University, Thailand.
Abstract
OBJECTIVE:
To evaluate the preventive effects of alkaline citrate on stone recurrence as well as stone growth post-ESWL or PCNL in patients with calcium-containing stones.
RESULTS:
At baseline, hypocitraturia was found in 20 of 39 patients (46.05%) of Group I and 15 of 37 patients (40.5%) of Group II. At 12 months, hypocitraturia was found in 3 of 39 (7.69%) and 14 of 37 (37.83%) of Group I and Group II, respectively (p = 0.007). At the 12 month follow-up, of the stone-free group, 92.3% of the treated group and 57.7% of the control group were still stone free. Of the residual stone group, 30.8% and 9.1% of treated and control group were stone-free, respectively. The increased stone size found in 7.7%) and 54.5%) of treated and control groups, respectively.
CONCLUSION:
Sodium-potassium citrate provides positive effects on stone-forming activities in calcium stone patients suffering from urolithiasis following treatment with ESWL and PCNL procedures at the 12-month follow-up
Duke Med Health News. 2008;Suppl:9.
Br J Nutr. 2008 Jun;99(6):1284-92. Epub 2007 Dec 6.
Braschi A, Naismith DJ.
Source
Department of Nutrition and Dietetics, King's College London, Franklin-Wilkins Building, 150 Stamford Street,
London SE1 9NN, UK.
Abstract
Blood pressure (BP) shows a continuous relationship with the risk of CVD. There is substantial evidence that dietary potassium exerts an anti-pressor effect. Most clinical trials have used KCl. However, the chloride ion may have a pressor effect and in foods potassium is associated with organic anions. In a double-blind randomized placebo-controlled trial we explored the effect on BP of two salts of potassium, KCl and potassium citrate (K-cit), in predominantly young healthy normotensive volunteers. The primary outcome was the change in mean arterial pressure as measured in a clinic setting. After 6 weeks of supplementation, compared with the placebo group (n 31), 30 mmol K-cit/d (n 28) changed mean arterial pressure by -5.22 mmHg (95% CI -8.85, -4.53) which did not differ significantly from that induced by KCl (n 26), -4.70 mmHg (-6.56, -2.84). The changes in systolic and diastolic BP were -6.69 (95% CI -8.85, -4.43) and -4.26 (95% CI -6.31, -2.21) mmHg with K-cit and -5.24 (95% CI -7.43, -3.06) and -4.30 (95% CI -6.39, -2.20) mmHg with KCl, and did not differ significantly between the two treatments. Changes in BP were not related to baseline urinary electrolytes. A greater treatment-related effect was observed in those with higher systolic BP. Increasing dietary potassium could therefore have a significant impact on the progressive rise in BP in the entire population.
Dtsch Med Wochenschr. 1995 May 5;120(18):631-5.
[Article in German]
Overlack A, Maus B, Ruppert M, Lennarz M, Kolloch R, Stumpe KO.
Source
Medizinische Universitäts-Poliklinik Bonn.
Abstract
A study was conducted on 25 patients (18 men, seven women; mean age 48 [24-70] years) with essential hypertension (EH) to see whether an increase in potassium supply influences blood pressure as well as metabolic and hormonal parameters, and whether the anion administered together with potassium affects the results. In a randomized, cross-over trial sequence the patients daily received 120 mmol potassium chloride, 120 mmol potassium citrate or a placebo, each for 8 weeks. Between each of the three periods there was a "wash-out" phase of 4 weeks each. After 8 weeks of potassium citrate intake the systolic and diastolic pressures were reduced significantly, by a mean of 6.2/3.8 mm Hg (P < 0.05). But after potassium chloride there was only a small, not significant, reduction. Metabolic and hormonal parameters (fasting glucose concentration, glucose tolerance test, lipid electrophoresis; plasma renin activity, plasma concentration of aldosterone, noradrenaline and insulin) were not significantly changed.--These findings suggest that an increased supply of potassium has a favourable haemodynamic effect, but this varies markedly between different potassium salts. An increase in potassium supply should thus be considered as an additional measure in the treatment of EH. As long as renal function is normal no unfavourable metabolic effect need be feared.
J Endourol. 2012 Apr 13. [Epub ahead of print]
Baia LD, Baxmann AC, Moreira SR, Holmes RP, Heilberg IP.
Source
Universidade Federal de São Paulo, Nephrology, Rua Botucatu, 740 , Vila Clementino , São Paulo, Brazil,
04023-900 , +55 (11) 5904-1697 ; leandronut@yahoo.com.br.
Abstract
Background and aims: Fruits and vegetables are natural suppliers of potassium, bicarbonate or bicarbonate precursors such as citrate, malate and others, hence possessing potential effects on citraturia. We aimed to compare the acute effects of a non-citrus (melon) fruit versus citric ones (orange and lime) upon citraturia and other lithogenic parameters. Methods: Two-hour urine samples were collected from 30 hypocitraturic stone-forming patients after an overnight fast and 2, 4 and 6 hours following the consumption of 385ml (13oz) of either freshly squeezed Orange juice (n=10), freshly blended Melon juice (n=10) or freshly squeezed Lime juice (n=10). Urinary citrate, potassium, pH and other lithogenic parameters were determined and Net Gastrointestinal Alkali Absorption (NGIA) was calculated. Potential Renal Acid Load (PRAL) and pH from juices were determined. Results: Significant and comparable increases on mean urinary citrate were observed in all groups, whereas mean urinary potassium, pH and NGIA were significantly increased only after consumption of Melon and Orange juices. The pH of Melon juice was higher and the PRAL value was more negative compared to Orange juice indicating a higher alkalinity. Conclusions: These findings suggested that Melon, a non-citrus source of potassium, citrate and malate, yielded an increase in urinary citrate excretion equivalent to that provided by Orange, and hence represents another dietary alternative for the treatment of hypocitraturic stone-formers. Despite its low potassium content, lime also produced comparable increases in citraturia possibly due to its high citric acid content. Keywords: kidney stones, nephrolithiasis, urinary citrate, potassium, alkalinization.
Antimicrob Agents Chemother. 2002 Jul;46(7):2077-86.
Cíftçíoglu N, Miller-Hjelle MA, Hjelle JT, Kajander EO.
Source
Department of Biochemistry, University of Kuopio, FIN-70211, Kuopio, Finland.
Abstract
Compounds from 16 classes of antimicrobial drugs were tested for their abilities to inhibit the in vitro multiplication of nanobacteria (NB), a newly discovered infectious agent found in human kidney stones and kidney cyst fluids from patients with polycystic kidney disease (PKD). Because NB form surface calcifications at physiologic levels of calcium and phosphate, they have been hypothesized to mediate the formation of tissue calcifications. We describe a modified microdilution inhibitory test that accommodates the unique growth conditions and long multiplication times of NB. This modified microdilution method included inoculation of 96-well plates and determination of inhibition by periodic measurement of the absorbance for 14 days in cell culture medium under cell culture conditions. Bactericidal or bacteriostatic drug effects were distinguished by subsequent subculture in drug-free media and monitoring for increasing absorbance. NB isolated from fetal bovine serum (FBS) were inhibited by tetracycline HCl, nitrofurantoin, trimethoprim, trimethoprim-sulfamethoxazole, and ampicillin at levels achievable in serum and urine; all drugs except ampicillin were cidal. Tetracycline also inhibited multiplication of isolates of NB from human kidney stones and kidney cyst fluids from patients with PKD. The other antibiotics tested against FBS-derived NB either had no effect or exhibited an inhibitory concentration above clinically achievable levels; the aminoglycosides and vancomycin were bacteriostatic. Antibiotic-induced morphological changes to NB were observed by electron microscopy. Bisphosphonates, aminocaproic acid, potassium citrate-citric acid solutions, and 5-fluorouracil also inhibited the multiplication of NB in a cidal manner. Insights into the nature of NB, the action(s) of these drugs, and the role of NB in calcifying diseases may be gained by exploiting this in vitro inhibition test system.
J Endourol. 2012 Apr 13. [Epub ahead of print]
Baia LD, Baxmann AC, Moreira SR, Holmes RP, Heilberg IP.
Source
Universidade Federal de São Paulo, Nephrology, Rua Botucatu, 740 , Vila Clementino São Paulo, Brazil, 04023-900
Abstract
Background and aims: Fruits and vegetables are natural suppliers of potassium, bicarbonate or bicarbonate precursors such as citrate, malate and others, hence possessing potential effects on citraturia. We aimed to compare the acute effects of a non-citrus (melon) fruit versus citric ones (orange and lime) upon citraturia and other lithogenic parameters. Methods: Two-hour urine samples were collected from 30 hypocitraturic stone-forming patients after an overnight fast and 2, 4 and 6 hours following the consumption of 385ml (13oz) of either freshly squeezed Orange juice (n=10), freshly blended Melon juice (n=10) or freshly squeezed Lime juice (n=10). Urinary citrate, potassium, pH and other lithogenic parameters were determined and Net Gastrointestinal Alkali Absorption (NGIA) was calculated. Potential Renal Acid Load (PRAL) and pH from juices were determined. Results: Significant and comparable increases on mean urinary citrate were observed in all groups, whereas mean urinary potassium, pH and NGIA were significantly increased only after consumption of Melon and Orange juices. The pH of Melon juice was higher and the PRAL value was more negative compared to Orange juice indicating a higher alkalinity. Conclusions: These findings suggested that Melon, a non-citrus source of potassium, citrate and malate, yielded an increase in urinary citrate excretion equivalent to that provided by Orange, and hence represents another dietary alternative for the treatment of hypocitraturic stone-formers. Despite its low potassium content, lime also produced comparable increases in citraturia possibly due to its high citric acid content. Keywords: kidney stones, nephrolithiasis, urinary citrate, potassium, alkalinization.
Familiarize yourself with the symptoms of high and low serum potassium.
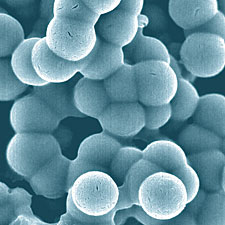
Nano Particle: Buffering System